Uterine Artery Embolisation
Fibroids are benign overgrowths of the uterus which are very common and may not cause problems, but if they become large or numerous, can result in painful symptoms.
Uterine artery embolisation is a procedure in which interventional radiologists can pass a fine tube (catheter) into the blood vessels supplying the uterus (uterine arteries)
and inject some fluid containing very small particles (embolic material) in order to block the small arteries and starve the fibroids of their blood supply. This makes the fibroids shrink significantly.
How will I benefit from UAE?
About 80% of women report a significant improvement in their quality of life and symptoms one year after the procedure. Some women have the procedure as they wish to try to get pregnant; in this case, you should seek advice from your fertility consultant, as they may advise you to not get pregnant for six months following the procedure.
How should I prepare before the
procedure?
You should inform your doctor about which medications you take, as some may need to be stopped or reduced. You may be asked to have some routine blood tests or more scans before the procedure. You need to let your team know if you have an IUD (intrauterine device or “coil”). You may be required to fast before the procedure.
The Procedure
A nurse will check your vital signs, and the team will place a small needle (cannula) in your arm so that you can be given medications in your vein. In many hospitals, a syringe containing pain-relieving and anti-nausea medications will be connected to the cannula and attached to a pump, so that you can deliver pain medications to yourself
by pressing a button during and after the procedure. This is known as Patient Controlled Analgesia – PCA. It is not possible to overdose oneself with these devices. In addition, at the start of the procedure, you may be given an intravenous sedative or tranquilliser to help you relax.
The doctor or nurse will clean your groin with antiseptic solution and cover you with sterile drapes. After giving local anaesthetic into your groin or wrist, the doctor will then insert a needle into the artery and feed a soft tube or catheter into the uterine artery on each side in turn, guided by the image on the x-ray screen. The doctor may be able to reach each uterine artery from one groin only, or might need to puncture the artery in the other groin.
Once the doctor is confident that they have placed the catheter in the correct position in the uterine artery, they will inject the embolic material. While this embolisation is going on and for several hours afterwards you may experience severe cramping pain.
The doctors and nurses will give you strong painkillers for this, usually via the cannula in your arm, and occasionally your rectum. If you have a PCA, you can deliver your own medications (you cannot overdose).
The procedure takes about an hour to perform. When the doctor has finished, they will remove the tube and press on your groin until any bleeding has stopped. You will need to keep your legs still and lie flat for 4 hours afterwards to let the puncture site recover quickly and prevent bleeding.
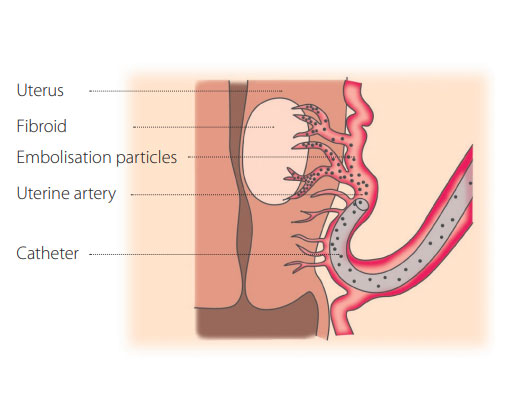
Catheter delivering embolisation particles
What are the risks?
Infection occurs in up to 2% of patients. The signs are severe pain, pelvic tenderness and a high temperature. Most infections can be treated with antibiotics. Extremely rarely, if infection is very severe, an operation to remove the womb (hysterectomy) may be required.
2–4% of women, especially those above 45, experience early menopause. Most women find it takes about six to nine months to resume regular periods.
What should I expect after the procedure?
What is the follow-up plan?
Once on the ward, the nurses will monitor you. Once you are able to eat and drink, walk around, go to the toilet without help, and control your pain with oral medication, you will be allowed home. Some women do need to stay in hospital longer than 24 hours. When you go home you are advised to rest for a few days. Most patients feel some pain afterwards, which can range from very mild to severe cramps. You will likely also have a slight fever; which is entirely expected in the first 24-72 hours.
Pain and fever can be controlled by oral painkillers and anti-fever medications. Pain and fever can be controlled by oral painkillers and anti-fever medications. Vaginal discharge can occur afterwards due to the fibroid breaking down. This can persist for up to two weeks or can be intermittent for a few months. If the discharge becomes smelly, and is associated with a fever, there is the possibility of infection and you should see your doctor urgently.
The interventional radiology or gynaecology team may arrange to follow up with you in about 4-6 weeks, and you may have another MRI or ultrasound scan after 6-9 months to
assess the effect of the embolisation.
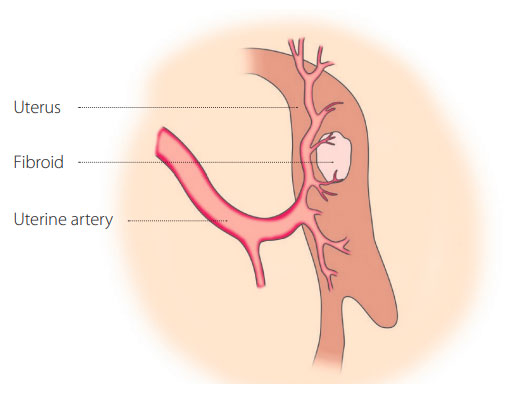
After embolisation, the fibroid will begin to break down.
